A patient recovering from COVID-19 is treated at the Casciana thermal baths spa, which has opened as a rehabilitation centre using its thermal water as part of treatment to help with respiratory difficulties, in Pisa, Italy, on Feb. 23, 2021.JENNIFER LORENZINI/Reuters
Raphael Rush is clinical director of Complex and Continuing Care at the Salvation Army-Toronto Grace Hospital.
Early in the pandemic, a patient sketched a picture of me on the back of a hospital menu. The figure, whom he named “Dr. Tomorrow,” looked sinister: a skinny silhouette in a pinstriped gown, a swooping polycarbonate visor hiding the mask beneath. Only a pair of tired eyes showed through the face shield I have worn almost every day for the past year as the doctor on my hospital ward, a rehabilitation unit for patients recovering from COVID-19.
Every day, intensive care units across Canada fill with new COVID patients. Although steroids and anti-inflammatory therapies have saved countless lives, none of these can prevent what happens next. Most of my patients entered the hospital otherwise healthy and independent; few will leave that way. Their recovery requires the resources of governments and the careful attention of doctors, nurses and therapists, all of which are in short supply.
As the pandemic wanes, hospitals must open more rehabilitation beds. Governments must expand access to outpatient therapy. But adding capacity indiscriminately will not be enough. Health care providers are going to have to find new models for rehabilitation both in hospitals and when patients return home, which means listening to what our patients are going to teach us about this still-new disease.
Each morning, I weave along the freshly-waxed linoleum around men and women standing for the first time in weeks. As I massage blobs of hand sanitizer into my cracked palms, I bear witness to the findings of a recent study that reported that fewer than half of the COVID patients admitted to intensive care units leave the hospital fully independent.
Many convalesce in rehabilitation hospitals like mine for months afterward. Some still breathe through surgical holes in their neck while they learn to walk again. Feeding solutions pumped into their stomachs supplement what little they can swallow. Our rehab nurses administer IV steroids and antiviral medications. Our therapists stand them up, teach them to walk and adjust the dials on the dull silver canisters of oxygen they still need to breathe.
The patients recovering from the third wave are younger and sicker than ever before. Time and again, the team on the ward rises to the occasion. By the time I hurry into the room where a man’s blood pressure has dropped one morning, his nurse has already hung an IV bag draining saline solution into his veins. I hook my fingers into the hollow of the wrist of a woman and feel her rapid pulse, while our pharmacist has already drawn the medication that will reset its rhythm. A physical therapist notices a patient’s wavy gait and diagnoses a stroke. At a cardiac arrest, our CEO, a respiratory therapist, hides his suit and tie beneath a surgical gown and slides a curved endotracheal tube between blue lips.
But even though they are sicker than ever before, patients spend less time on our ward than they would have before the pandemic began. The third wave’s full ICUs have exacerbated a chronic shortage of Canada’s scarce rehabilitation beds. And the longer patients wait without rehab, the worse they do once they arrive. Waiting for rehabilitation has the same impact on COVID survivors as it does on anyone who enters the ICU. The longer ICU survivors lie in bed awaiting therapy, the more muscle mass they lose: Long waits themselves can therefore cause permanent yet preventable disability.
So discharge is rarely the end of each survivor’s journey; it’s usually just the beginning. And many patients want to leave early. A man reminds me that he missed winter this year and doesn’t intend to miss spring. He can’t wait to feel the wind ruffle the hairs on his arms, even if he still stumbles over his walker. Other patients simply tire of months of windowless rooms and hospital food. Another woman is the caregiver for elderly parents who have survived COVID in an earlier wave. Although she still needs care herself, she is sure they need it more.
Our social workers work overtime to find nurses who can visit patients at home and dress hollow ulcers or inject syringes of insulin. They hire personal support workers, essential workers to tend to the essential workers who comprise many of my patients, whom I cannot help but think we have failed.
I worry about my patients even after they leave. In Ontario, many patients receive daily therapy sessions as long as they remain in hospital. When they return home, they typically receive between six and 14 sessions in total. For patients with other diseases, this sometimes suffices. But the effects of COVID persist for months, and we still don’t know how to best rehabilitate its survivors.
Often, I scribble a prescription for therapy, hoping that a patient might have private insurance which covers the balance. But other times, I am stuck haplessly recommending YouTube rehab videos targeted toward patients with different diseases, and promising that someone will see them in clinic, hoping they will have found a way to strengthen themselves.
I meet my patients again weeks or months later in clinic. No matter how well they have done, recovery from COVID continues long after patients leave hospital. Many still struggle to stand up every morning. They still miss the smells of pine needles or hamburgers. People grown old before their time stoop over walkers. Behind their masks, many still cough.
In the room across the hall from my clinic, a respiratory therapist, her face half-hidden by the clamshell of her N95 mask, urges patients to blow into a tube. The other doctors in the clinic and I can assess lung function, prescribe inhalers, and order CAT scans to detect residual damage, but only patients themselves show us what we’re really looking for: when it will all end; maps guiding them back to themselves.
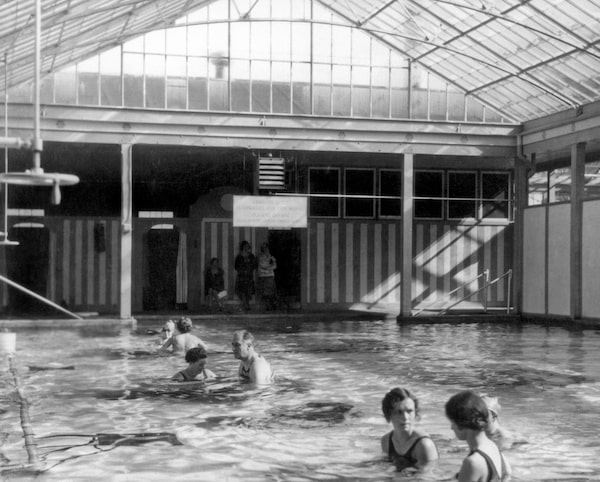
Franklin Roosevelt exercises his polio damaged legs in the enclosed pool, Warm Springs, Ga., 1928.Underwood Archives/Getty Images
Survivors themselves will teach us how to heal. It’s a lesson I learned from many of my patients even before the pandemic began, and particularly from survivors of the polio epidemics which afflicted millions during the first half of the 20th century. The vaccines of the late 1950s arrived too late for millions who were permanently paralyzed. Most of their doctors once assumed that patients’ lives and clinical courses ended at the moment of diagnosis.
But the survivors proved otherwise. Franklin Delano Roosevelt, who contracted polio in 1921, ignored his surgeon’s advice to rest in bed for months. After discovering that swimming eased his pain and strengthened his muscles, he bought an inn in Warm Springs, Ga., which he converted into one of North America’s first rehabilitation institutions for polio survivors.
Survivors were encouraged to live normal lives. They set goals for themselves, including the core set of activities that form the nucleus of modern rehabilitation known as the activities of daily living. Physicians and therapists trained them to use bathtubs and toilets, to clean and to cook, and helped them live in a world still sometimes hostile to their existence by modifying swimming pools with features which allowed survivors to swim safely with paralyzed limbs and installing ramps to make each building accessible.
The polio outbreaks of the following decade taxed Roosevelt’s personal finances as the facility accommodated more patients. He established the National Foundation for Infantile Paralysis, later known as the March of Dimes, to fund its expansion and recruit staff. Some of the new doctors, nurses and therapists were once patients themselves. These former patients developed new therapy techniques from personal experience. Survivors encouraged each other to direct their own lives and set priorities for the institution and for themselves, a model of care from which we can still learn today.
After the inhaler training and CAT scan reports, after my questions and their answers, my patients explain how they have surpassed or adapted to their physical limitations. I am often pleasantly surprised to hear about their new jobs, early retirements or new hobbies. Some teach me forms of therapy they discovered themselves: breathing exercises; puzzles they solve to help regain mental acuity; essential oils they’ve collected to retrain a diminished sense of smell. And they describe the treatments and therapies they still need. Some are unfunded. Others don’t yet exist. Individually, they try to solve their own problems. Collectively, they look like a movement. The health care system must follow their lead.
The first waves of the pandemic prompted the discovery of new therapies to treat COVID and vaccines to prevent it. As the final waves ebb, researchers and health care workers must learn how to rehabilitate the damage the virus has dealt its survivors. In the coming months, hospitals and governments will fund programs to treat these survivors. They will open more beds, and hopefully open new outpatient programs. They will reach out to doctors, therapists, administrators and countless other health care professionals in an effort to find out which programs are needed. But they will have to engage patients as well.
COVID’s survivors will teach us which existing forms of therapy to fund; which new therapies work; and which medical and personal outcomes matter most. They will teach us what recovery means.
Keep your Opinions sharp and informed. Get the Opinion newsletter. Sign up today.